Introduction
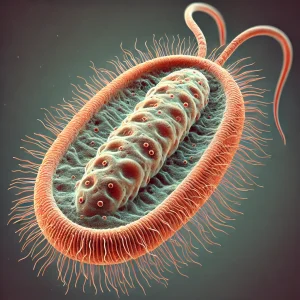
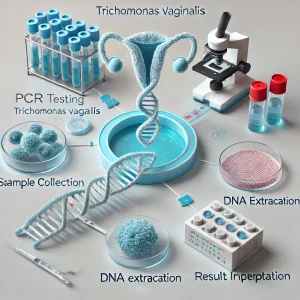
Trichomonas vaginalis (T. vaginalis) is a common sexually transmitted infection (STI) that can cause significant reproductive health issues. Polymerase Chain Reaction (PCR) is widely used for the detection of T. vaginalis due to its high sensitivity and specificity. Ensuring positive quality control (QC) in PCR testing is essential for accurate diagnosis and treatment. Several regulatory agencies, including the Centers for Disease Control and Prevention (CDC), World Health Organization (WHO), and Food and Drug Administration (FDA), provide guidelines for effective quality control in molecular diagnostics.
Importance of Quality Control in T. vaginalis PCR Testing
Effective quality control ensures that PCR testing for T. vaginalis is accurate, reproducible, and free from contamination. External and internal QC measures are necessary to avoid false positives and negatives. Organizations like the CDC and WHO offer best practices for laboratory diagnostics (CDC Laboratory Quality Assurance, WHO Laboratory Standards).
Key Components of Positive Quality Control
1. Reference Materials and Standards
- WHO-approved reference strains ensure proper assay validation (WHO Reference Standards).
- The National Institute of Standards and Technology (NIST) provides certified nucleic acid reference materials (NIST Reference Materials).
- External proficiency testing (PT) programs are essential for accreditation (CAP Proficiency Testing).
2. Sample Collection & Processing
- Proper specimen collection techniques prevent degradation and contamination (CDC Specimen Collection Guidelines).
- Maintaining optimal storage conditions is crucial for RNA/DNA integrity (FDA Storage Recommendations).
- WHO provides best practices for transport media and handling procedures (WHO Laboratory Testing Standards).
3. PCR Assay Validation & Calibration
- Assay validation ensures accurate amplification of T. vaginalis DNA (FDA PCR Validation Guidelines).
- PCR instruments must undergo regular calibration and verification to maintain accuracy (CDC PCR Instrument Calibration).
- Internal controls, such as positive and negative controls, must be included in every PCR run (CLIA Quality Control Guidelines).
4. External Proficiency Testing
- Proficiency testing (PT) ensures consistent detection of T. vaginalis across laboratories (CAP Proficiency Testing).
- Interlaboratory comparison studies improve testing reliability (WHO EQA Programs).
- National External Quality Assessment Service (NEQAS) provides independent assessment of test performance (NEQAS Guidelines).
Challenges in T. vaginalis PCR Quality Control
- Genetic Variability: Some T. vaginalis strains exhibit mutations affecting primer binding (CDC Trichomonas Genetic Research).
- Cross-contamination Risks: Preventing laboratory contamination is crucial for maintaining accurate results (FDA Contamination Prevention).
- Reagent Lot Variability: Using validated reagents ensures consistency across multiple runs (NIH Reagent Quality Control).
Regulatory Compliance and Accreditation
- Clinical Laboratory Improvement Amendments (CLIA) sets molecular diagnostic standards (CMS CLIA Regulations).
- FDA oversees the validation and approval of molecular diagnostic assays (FDA IVD Regulations).
- WHO provides laboratory guidelines for diagnostic quality assurance (WHO Laboratory Accreditation).
- International Organization for Standardization (ISO 15189) establishes best practices for medical laboratories (ISO 15189 Standards).
Future Innovations in T. vaginalis PCR Quality Control
- Next-Generation Sequencing (NGS) to enhance pathogen detection (NIH NGS Research).
- Artificial Intelligence (AI) in PCR Data Analysis for improved diagnostic accuracy (FDA AI in Diagnostics).
- Automated Quality Control Systems to minimize human error (CDC Automated Laboratory Testing).
- Multiplex PCR Assays for detecting multiple STIs, including T. vaginalis, Chlamydia, and Gonorrhea (NIH Multiplex PCR Testing).
Conclusion
Best Practices for Quality Control in Trichomonas vaginalis PCR Testing is crucial for ensuring reliable and accurate diagnostic results. Adhering to best practices outlined by CDC, WHO, FDA, CLIA, and ISO ensures the highest laboratory testing standards. Ongoing advancements in automation, AI-driven diagnostics, and NGS technologies will further enhance the precision of T. vaginalis PCR testing, contributing to improved public health and STI surveillance worldwide.